By: Faisal Latif, MD, FSCAI and Suresh Mulukutla, MD, FSCAI
Peri-procedural bleeding is associated with increased short- and long-term morbidity and mortality in addition to increased costs. Patients at particularly increased risk include the elderly, those who are undergoing emergent procedures, those with either very low or very high BMI, and those with chronic kidney disease. Evidence-based strategies to reduce bleeding events may include using –
- the radial approach for PCI,
- bivalirudin, and/or
- femoral vascular closure devices.
However, there is a well-described "risk-treatment" paradox, whereby bleeding avoidance strategies are predominantly used in patients at lower risk instead of in patients at the highest risk of bleeding.1
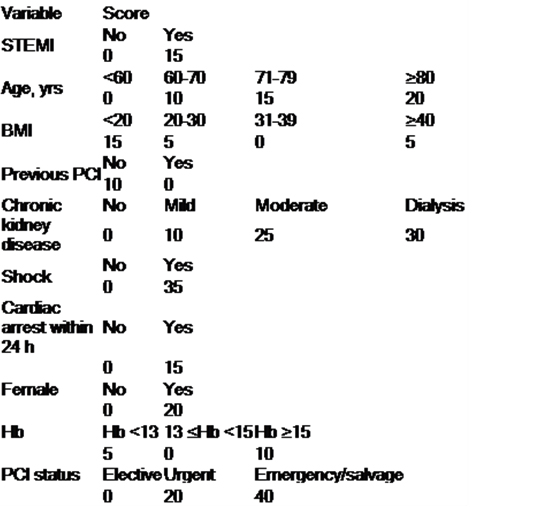
Risk prediction for bleeding can be easy! Use a simplified scoring system to assess bleeding risk (see Table below)2 and the aforementioned tactics to minimize bleeding. Scores <25 are considered low (<2%); 25-65, intermediate (2-6%); and >65 are considered high (>6.5%) for risk of bleeding.
Stay tuned for the SCAI PCI Risk Assessment Tool, which will be at your fingertips soon! You can always retrospectively analyze your performance using the NCDR database.
Table
References
Marso S.P., Amin A.P., House J.A., et al. Association between use of bleeding avoidance strategies and risk of periprocedural bleeding among patients undergoing percutaneous coronary intervention. JAMA. 2010;303:2156-2164.
Rao SV, McCoy LA, Spertus JA, et al. An Updated Bleeding Model to Predict the Risk of Post-Procedure Bleeding Among Patients Undergoing Percutaneous Coronary Intervention: A Report Using an Expanded Bleeding Definition From the National Cardiovascular Data Registry CathPCI Registry. J Am Coll Cardiol Intv. 2013;6(9):897-904.
Related QI Tips
Other evidence-based methods and tools you can use to improve quality of care and outcomes for patients.
