Rahul Sawhney, DO; Srini Potluri, MD, FSCAI; Faisal Latif, MD, FSCAI
Introduction
As interventional cardiologists, we have some of the highest exposures to ionizing radiation across all medical specialties. There are several shielding mechanisms, but they have their own drawbacks, including orthopedic problems, gaps in coverage, cost, etc.
In this Tip of the Month, we focus on best practices for radiation safety, ways to reduce radiation exposure, and new technologies that can help mitigate these risks.
Practical Pointers
- Protection starts with avoidance. The ALARA—as low as reasonably achievable—principle calls for reducing radiation to the patient, operator, and staff.1
- Patient and operator exposure should be minimized. Less radiation for the patient = less radiation for the operator.1-2
- Optimize the area being irradiating (focus on what is important).
- Collimate and optimize the table position over the area of interest.
- Maximize the distance between the X-ray tube and the patient’s skin.
- Raise the table height to reduce scatter by bringing the patient closer to the image intensifier and ensure that there is adequate shielding under the table.
- Minimize the distance between the image intensifier and the patient’s skin, as this reduces scatter radiation.
- Reduce frame rates to 7.5 frames per second for fluoro and 15 for cine.
- Ensure that preferred X-ray settings are configured prior to starting the case (especially for complex interventions).
- Use software zoom instead of hardware magnification.
- Avoid steep angles to reduce both scatter and leakage.
- Change the C-arm angle to avoid prolonged radiation to the same area.
- Delay staged procedures to allow for skin healing.
- Optimize the area being irradiating (focus on what is important).
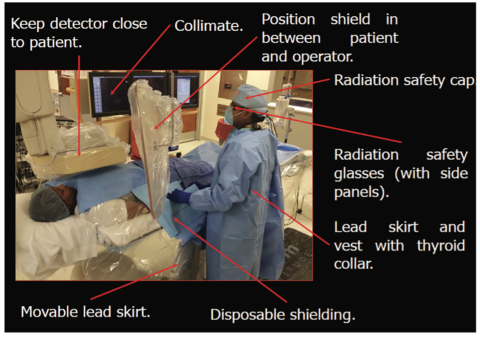
- Appropriate personal shielding should be utilized.1-2
- Lead aprons (with thyroid collar and ideally with underlying back support)
- A lead-equivalent minimum, front and back, of 0.25 mm (the standard is 0.5 mm)
- Lead glasses/goggles3-5
- A total of 95% ocular radiation reduction
- Utilization of a side shield design, which offers better protection
- Radiation shielding pads/hats3-5, 10
- Radiation pads: A significant reduction for the operator without significant increase for the patient
- Radiation hats: A reduction of exposure to the skull (but no evidence of the prevention of brain tumors)
- Table skirts/shields
- No large gaps
- Boom-mounted and portable shields
- Appropriate positioning
- Lead aprons (with thyroid collar and ideally with underlying back support)
- Personnel should stay as far away as possible from the X-ray source.1-2
- Manifold extension tubing or an auto-injector system (e.g. ACIST, MedRad, etc.) should be used.
- Cranial angulations increase operator exposure due to proximity to the x-ray source
- The left anterior oblique (LAO) cranial has the highest scatter exposure for the operator.
- Exposure decreases exponentially with each step away from the source
- When the distance is doubled, the exposure is reduced by a factor of four.
- Hands, feet, and other objects should be kept to yourself (and out of the X-ray beam).
- Digital subtraction angiography (DSA) should be used judiciously during peripheral procedures.6-7
- DSA significantly increases radiation, but careful collimation and caudal angulation reduce exposure.
- Operator/staff should maximize their distance away from the source during DSA runs.
- Patients with peripheral artery disease (PAD) are subjected to more frequent DSA exposure given the recurrence of disease.
- Personal dosimetry monitors should be worn by all operators and staff.1-2
- Pregnant people should wear double aprons and have a separate dosimeter at waist level.
- Staff should remind operators of dose thresholds and remain mindful of the fluoroscopy timer.1-2
- A radiation quality assurance program should be established and followed.1-2
- Documentation and skin follow-up for patient exposures > 5 Gy
- A medical physicist’s review for exposures > 10 Gy
- A joint review of cases with > 15 Gy exposure (considered a Joint Commission sentinel event)
- Audit radiation safety practices of the operators/staff with the highest exposure
- Per U.S. law, the limitation of a radiation worker’s total body exposure to 50 mSv annually (20 mSv in Europe)
- Inspection of lead aprons for damage at least annually
- Documentation and skin follow-up for patient exposures > 5 Gy
- New shielding technologies should be considered, if feasible.3, 8
- More patient-focused shielding (shielding applied to the camera/table and/or source/receiver), which reduces scatter/leakage and benefits everyone in the cath lab (e.g., Eggnest, Radiaction)
- Lead “replacement” systems (ceiling-/boom-mounted shielding/apron equivalent that transfers weight off the operator), which primarily reduce exposure for the operator (e.g., Zero Gravity)
- Lead “isolation” systems, which isolate radiation on the side of the patient only and reduce scatter/leakage to the benefit of all personnel in the room (e.g., Rampart, Protego)
Figure 1: Summary diagram of best practices for radiation reduction.9
Summary
- The best protection is avoidance (remember ALARA—“as low as reasonably achievable”).
- Fluoro time should be minimized, the distance from the radiation source should be maximized, and shielding should be used in a smart manner.
- Ergonomics are just as important as radiation protection.
References
- Chambers CE, Fetterly KA, Holzer R, et al. Radiation safety program for the cardiac catheterization laboratory. Catheter Cardiovasc Interv. 2011 Mar 1; 77(4): 546-56.
- Christopoulos G, Makke L, Christakopoulos G, et al. Optimizing Radiation Safety in the Cardiac Catheterization Laboratory: A Practical Approach. Catheter Cardiovasc Interv. 2016 Feb 1; 87(2): 291-301.
- Vlastra W, Delewi R, Sjauw KD, et al. Efficacy of the RADPAD Protection Drape in Reducing Operators’ Radiation Exposure in the Catheterization Laboratory: A Sham-Controlled Randomized Trial. Circ Cardiovasc Interv. 2017 Nov; 10(11): e006058.
- Kern M. Novel Radiation Protection Devices: An Update on Radiation Safety in the Cath Lab. Cath Lab Digest, January 2018. Accessed November 1, 2023. https://www.hmpgloballearningnetwork.com/site/cathlab/article/novel-radiation-protection-devices-update-radiation-safety-cath-lab.
- Biso SMR, Vidovich MI. Radiation protection in the cardiac catheterization laboratory. J Thorac Dis. 2020 Apr; 12(4): 1648-55.
- Haqqani OP, Agarwal PK, Halin NM, et al. Minimizing radiation exposure to the vascular surgeon. J Vasc Surg. 2012 Mar; 55(3): 799-805.
- Meisinger QC, Stahl CM, Andre MP, et al. Radiation Protection for the Fluoroscopy Operator and Staff. AJR Am J Roentgenol. 2016 Oct; 207(4): 745-54.
- Pristera N, Chung CJ. Essential Strategies to Optimizing Radiation Safety Training for Fellows and Cath Lab Staff. Cardiac Interventions Today, 2023. Accessed November 1, 2023. https://citoday.com/articles/2023-digital-exclusive-1/essential-strategies-to-optimizing-radiation-safety-training-for-fellows-and-cath-lab-staff.
- Kumar G, Rab ST. Radiation Safety for the Interventional Cardiologist—A Practical Approach to Protecting Ourselves From the Dangers of Ionizing Radiation. American College of Cardiology, January 4, 2016. Accessed November 1, 2023. https://www.acc.org/latest-in-cardiology/articles/2015/12/31/10/12/radiation-safety-for-the-interventional-cardiologist.
- Sattar Y, Sengodan PM, Cheema MS, et al. Lead Cap Use in Interventional Cardiology: Time to Protect Our Head in the Cardiac Catheterisation Laboratory? Interv Cardiol. 2023; 18: e18.
Related QI Tips
Other evidence-based methods and tools you can use to improve quality of care and outcomes for patients.