Prior authorization (PA) is a process where physicians and other medical care providers must obtain pre-approval for certain procedures and treatments from health insurance companies before rendering care to their patients. In recent years, this process has become increasingly dangerous for patients and burdensome for providers.
Insurance companies have repeatedly expanded the scope of services that require prior authorization, often delaying or denying care even when it is medically necessary.
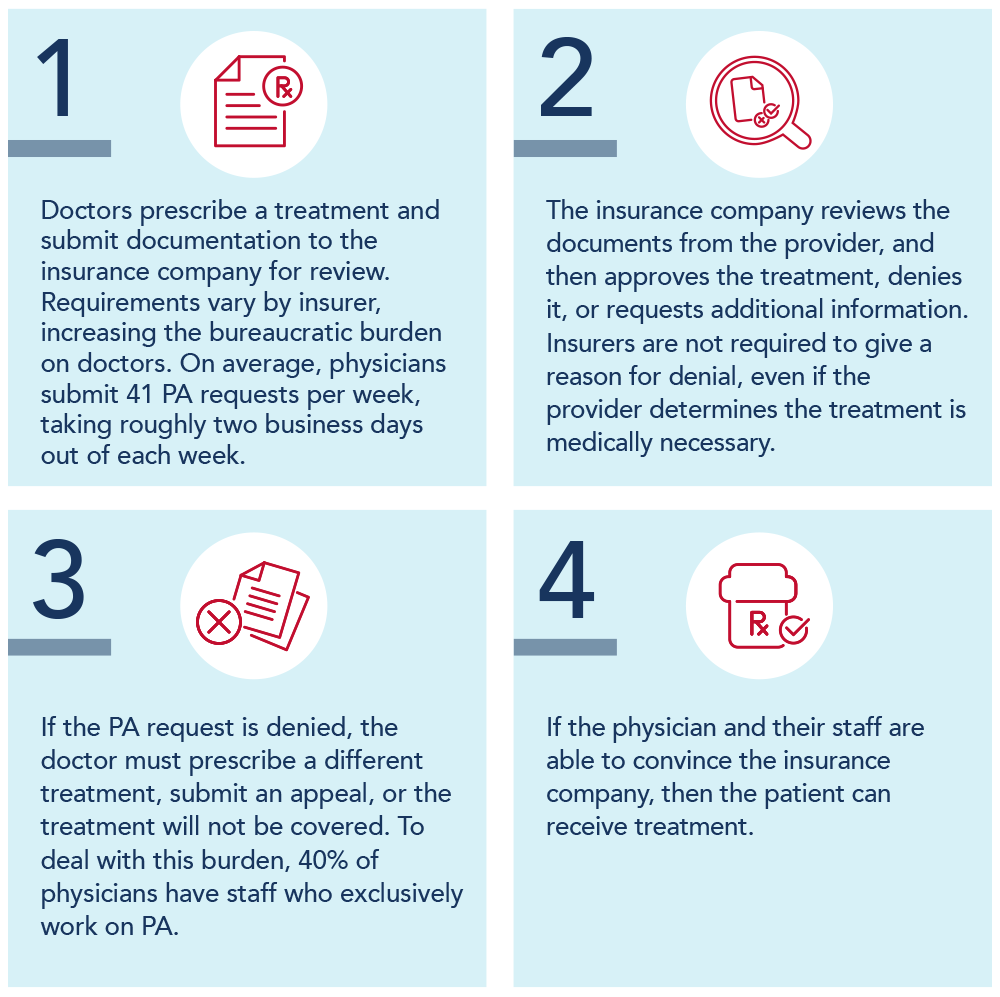
The Process
Patients Can Experience Delays of up to 3 Weeks Before Receiving PA Approval
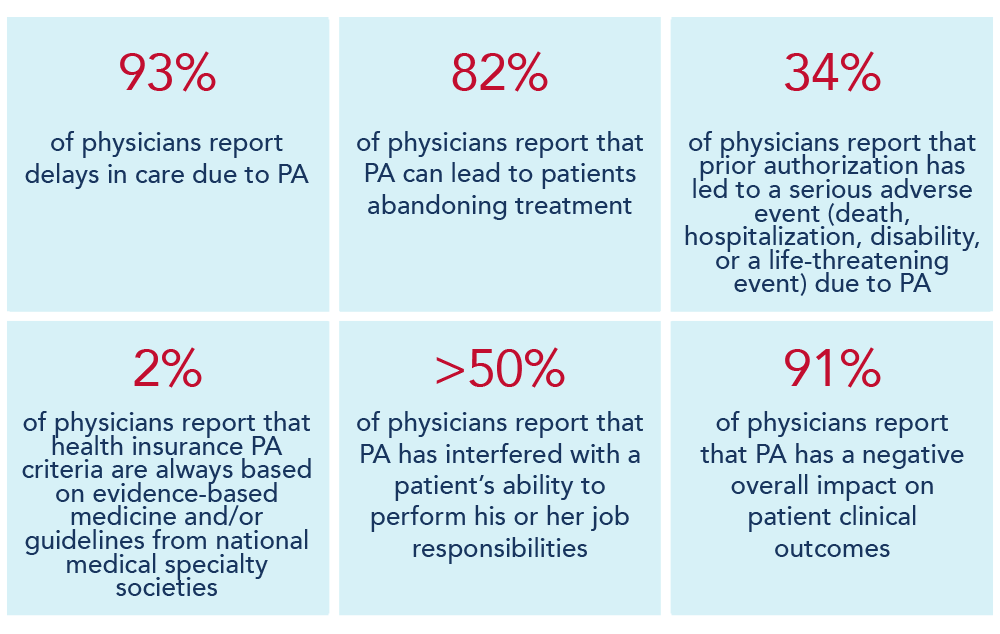
What Is the Impact on Providers and Patients?
How Can Congress Fix Prior Authorization?
Congress should codify the provisions of the proposed rule from the Centers for Medicare & Medicaid Services that would:
- Establish an electronic prior authorization (ePA) program and require MA plans to adopt ePA capabilities
- Require the Secretary of Health and Human Services to establish a list of items and services eligible for real-time decisions under an MA ePA program
- Standardize and streamline the prior authorization process for routinely approved items and services
- Ensure prior authorization requests are reviewed by qualified medical personnel
- Increase transparency around MA prior authorization requirements and their use
- Protect beneficiaries from any disruptions in care due to prior authorization requirements as they transition between MA plans.
Additionally, these requirements should be extended to private health insurers through Congressional action.
SCAI strongly supports the Improving Seniors' Timely Access to Care Act (S.4532/HR.8702) reintroduced on June 12th, 2024 by Senators Roger Marshall (R-KS), Kyrsten Sinema (I-AZ), John Thune (R-SD), Sherrod Brown (D-OH), and U.S. Representatives Mike Kelly (R-PA), Suzan DelBene (D-WA), Larry Bucshon, M.D. (R-IN), and Ami Bera, M.D. (D-CA).
The Improving Seniors Timely Access to Care Act will reduce the regulatory burden in Medicare Advantage by requiring any plan that imposes prior authorization requirements to be transparent about that requirement and to provide an electronic copy of what services required prior authorization during the prior year. The bill makes sure prior authorization requests are reviewed by a medical professional rather than through a machine or an algorithm. It also streamlines the prior authorization process for commonly approved items and services.