Introduction
Transcatheter patent ductus arteriosus (PDA) stenting (versus surgical shunts) is evolving as a preferred option for newborns with ductal dependent pulmonary blood flow. 1–4 The vascular access site is critical for procedure success. In general, arterial access with the straightest PDA access is favorable.4–7 Traditional ductal anatomy is typically amenable to a transfemoral approach. Vertical or tortuous PDAs are better accessed from a transaxillary or transcarotid approach. In this SCAI Tip of the Month, we present a step-by-step approach to choosing the correct access site for your patient.
Pre-Procedure Planning
- Carefully review the echocardiogram for basic anatomy.
- Consider a contrast-enhanced cardiac computed tomography (CT), ideally with 3D segmentation.
- Without advanced imaging, plan for catheterization to start with an aortogram (transfemoral or transumbilical artery) to determine the best PDA access site.
- PGE management:
- Single source PDAs: do not turn off the PGE
- Why?
- PDA is typically tortuous so will hold the stent even if it is not stenotic
- Avoids pre procedure compromise of pulmonary blood flow or intra-procedure PDA spasm
- Oxygen saturation = 80’s— >leave PGE at the same dose
- Oxygen saturation = mid 90’s— >lower the PGE to 0.01 mcg/kg/min
- Why?
- Dual source PDAs (PDA + prograde flow across the pulmonary valve; typically straighter and often approached from the femoral vein).
- Oxygen saturation = 90’s— >consider turning PGE off for lower oxygen saturations
- Check by echo for an area of stenosis in the PDA
- Single source PDAs: do not turn off the PGE
Access Site
- Identify if the PDA arises from the descending aorta or the undersurface of the aortic arch (Figure 1).
- Descending aorta— >transfemoral artery approach
- Undersurface of the aortic arch— >transaxillary or transcarotid arterial approach (Figure 2).
- Allows straightening of tortuous PDAs, which is a key for success.
- Transaxillary versus transcarotid (institutional and operator comfort).
- Right versus left axillary (typically, left aortic arch = left axillary and, right arch = right axillary; a CT can identify exceptions).
Procedural Considerations
- Table position:
- Transfemoral: Set up table preparation for a typical working position (groin).
- Transaxillary or transcarotid: Use a “head-up” approach (Figure 3) to allow more space for table set-up and catheter manipulation.
- Patient position/vascular access:
- Transaxillary (Figure 3): Position the arm either at 90 degrees or with the arm down close to the chest. The arterial puncture site is in the delto-pectoral groove just below the pectoralis minor. Use ultrasound guidance alone or in addition to a soft, low-profile wire target (introduced from additional transfemoral access) for additional image guidance and vessel stability.
- Transcarotid: Turn the neck to the opposite side of the artery being accessed. Use ultrasound guidance for targeting and avoiding a through-and-through puncture. A surgical cut-down may be used per institutional preference.
- Accessing the PDA:
- Use a 4F short sheath (5cm).
- Gently maneuver flexible, coaxial angled catheters (Renegade, Boston Scientific, Marlborough, MA; Glidecath, Terumo, Somerset, NJ) and soft wire (BMW, Abbott, Santa Clara, CA) across the PDA into main or branch pulmonary arteries.
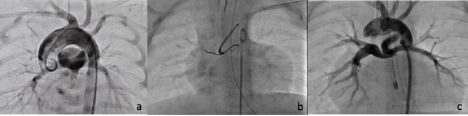
- Consider exchanging soft wire for stiffer wires (Thruway, Boston Scientific, Marlborough, MA or Ironman, Abbott, Santa Clara, CA), which straightens the PDA and allows ease of coronary stent trackability (Figure 4).
- Because stiffer wires can decrease PDA flow, emphasize the need for speed during this procedural step. Wire removal may cause a ductal spasm.
Conclusion
A thoughtful, step-wise approach to vascular access site choice dictates transcatheter PDA stenting success and procedural ease.
References
- Alwi M, Choo KK, Latiff HA, et al. Initial results and medium-term follow-up of stent implantation of patent ductus arteriosus in duct-dependent pulmonary circulation. J Am Coll Cardiol. 2004 Jul 21;44(2):438–45.
- Glatz AC, Petit CJ, Goldstein BH, et al. Comparison Between Patent Ductus Arteriosus Stent and Modified Blalock-Taussig Shunt as Palliation for Infants With Ductal-Dependent Pulmonary Blood Flow: Insights From the Congenital Catheterization Research Collaborative. Circulation. 2018 Feb 6;137(6):589–601.
- Bentham JR, Zava NK, Harrison WJ, et al. Duct Stenting Versus Modified Blalock-Taussig Shunt in Neonates With Duct-Dependent Pulmonary Blood Flow: Associations With Clinical Outcomes in a Multicenter National Study. Circulation. 2018 Feb 6;137(6):581–8.
- Ratnayaka K, Nageotte SJ, Moore JW, et al. Patent Ductus Arteriosus Stenting for All Ductal-Dependent Cyanotic Infants: Waning Use of Blalock-Taussig Shunts. Circ Cardiovasc Interv. 2021 Mar;14(3):e009520.
- Santoro G, Gaio G, Giugno L, et al. Ten-years, single-center experience with arterial duct stenting in duct-dependent pulmonary circulation: early results, learning-curve changes, and mid-term outcome. Catheter Cardiovasc Interv. 2015 Aug;86(2):249–57.
- Lee J, Ratnayaka K, Moore J, El-Said H. Stenting the vertical neonatal ductus arteriosus via the percutaneous axillary approach. Congenit Heart Dis. 2019 Sep;14(5):791–96.
- Bauser-Heaton H, Qureshi AM, Goldstein BH, et al. Use of carotid and axillary artery approach for stenting the patent ductus arteriosus in infants with ductal-dependent pulmonary blood flow: A multicenter study from the congenital catheterization research collaborative. Catheter Cardiovasc Interv. 2020 Mar 1;95(4):726–33.
Figure 1: (a) The PDA arises from the descending aorta and, thus, is easier to approach from the femoral artery. (b) The PDA arises from the undersurface of the arch and is easier to approach from the head and neck vessels.
Figure 2: (a) The origin of the PDA is angled to the left, so the left axillary is preferred. (b) Even with a left arch, the PDA origin can be angled to the right, so the right axillary is preferred.
Note that carotid access is typically in line with the origin of the PDA in either case.
Figure 3: (a) “Head-up” approach: The AP camera base is moved caudal, and the lateral camera is moved cephalad, allowing more room at the head of the bed. (b) Transaxillary access: This is an anatomical representation of the puncture site in the delto-pectoral groove. (c) This is the arm position for a left axillary approach with vascular sheath in place. (d) Wire target technique: Guidewire (transfemoral introduction) is positioned in the left axillary artery, and fluoroscopy guides the needle position and trajectory together with ultrasound. (e) Ultrasound depicts the typically superficial artery (arrow) and vein.
Figure 4: (a) The PDA is very tortuous with a 36-degree turn, arising from the undersurface of the arch. (b) The PDA has been straightened with a stiff wire. (c) The PDA stents is deployed, straightening the PDA with good flow to both branch pulmonary arteries.
Related QI Tips
Other evidence-based methods and tools you can use to improve quality of care and outcomes for patients.