Arka Chatterjee, MD, FSCAI; Faisal Latif, MD, FSCAI
Introduction
With widespread uptake of structural heart procedures, transseptal puncture (TSP) is now an essential part of the tool kit for interventional cardiologists. Complications are rare, in the range of 1%.1 However, they can be life-threatening; hence, it is essential to ensure safe TSP practices.
In this Tip of the Month (TOTM), we focus on safe TSP techniques using different settings. Handling all aspects of challenging TSPs are not in the scope of this TOTM.
Tips & Tricks
Any TSP starts with safe femoral venous access. Ultrasound-guided access is preferred. It may be useful to have a longer sheath with a larger diameter than the transseptal (TS) sheath if iliac tortuosity is present.
Fluoroscopic-Guided TSP
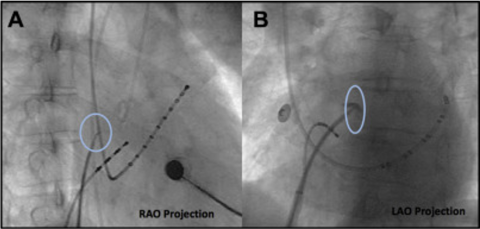
In this technique, the TS sheath (Mullins/SL1/others) is pulled down from the innominate vein or the super vena cava (SVC), and the jumps are observed until the sheath falls into the fossa. A pigtail catheter is usually maintained at the level of the aortic valve in the noncoronary cusp. Once the TS sheath is just below the pigtail catheter in the anterior-posterior (AP) or right anterior oblique (RAO) view, the angle is changed to left anterior oblique (LAO), and it is ensured that the sheath is pointing in between the pigtail catheter and the spinal column. Contrast staining can be performed if using a mechanical needle to ensure tenting of the fossa (Figure 1).2 TSP is then done and confirmed with a left atrial pressure tracing or contrast injection. The dilator and sheath are not advanced until the needle position in the left atrium is confirmed.
- Pros: This technique does not require extra personnel/equipment for imaging.
- Cons: If there is a cardiac chamber or aortic root enlargement, fluoroscopy may be misleading and can lead to an inadvertent puncture of the aorta or the atria, thus leading to hemopericardium.
Transesophageal Echocardiogram (TEE)-Guided TSP
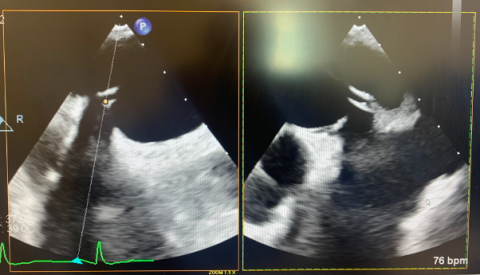
In a TEE-guided TSP, the TS sheath is dragged down from the SVC under TEE visualization; using X-plane TEE imaging is very helpful. As the sheath drops into the fossa ovalis, the X-plane is centered on the tenting of the septum in the bicaval view (showing the location of the TS sheath in the superior-inferior plane) with the orthogonal plane showing the position in the AP plane (Figure 2).
The position is adjusted, as needed, depending on the procedure being performed—going more posterior is usually achieved by putting a clockwise torque with a slight withdrawal; just applying torque will often cause a jump with the loss of position, thus necessitating the operator to start over. Moving more anterior is achieved with a counterclockwise torque.
- Pros: This technique is safer, and there is less chance of inadvertently puncturing atrial walls.
- Cons: This technique requires general anesthesia and a separate operator for the TEE.
Intracardiac Echocardiogram (ICE)-Guided TSP
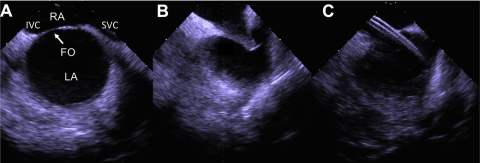
The challenge with doing an ICE-guided TSP is visualization in one plane only. Hence, position in the fossa is confirmed on the septal view followed by the short-axis view to confirm position in the AP axis (Figure 3). Another way to confirm proper positioning is observing left atrial structures. When only the left atrial appendage (LAA) is visible, this is an anterior location; visualizing the left pulmonary veins (PV) is a posterior puncture. If the plane moves beyond the left PVs, puncture is to be avoided.
- Pros: This technique requires no general anesthesia.
- Cons: This technique involves a steeper learning curve and additional vascular access.
Difficult Anatomies
Thick Septum/Prior Septoplasty
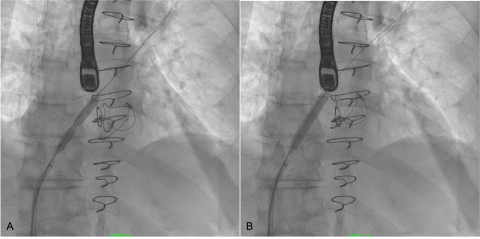
In this setting, mechanical needle-based systems tend to slip or buckle, so imaging is very essential to ensure an appropriate position. It is possible to have difficulty getting the dilator and sheath to cross— if the needle crosses over, a coronary wire can be advanced and serial balloon dilation can be performed. If the dilator crosses over, but the sheath will not advance, a 0.032’ stiff wire can be advanced into the PV and septostomy can be performed with a balloon (Figure 4) or with an Inoue dilator. If the needle itself does not cross, even with gentle torquing of the needle on the fossa, it can be facilitated by the back end of a coronary wire or with electrocautery applied to the proximal end of the BRK needle. Radiofrequency (RF) needle systems tend to cross over easier in this situation.
Prior Atrial Septal Defect (ASD)/Patent Foramen Ovale (PFO) Closure Device
In this setting, it may be possible to approach the puncture inferior and posterior to the implanted occluder or sometimes through the occluder.3 For the latter, balloon dilation or serial dilation may be required. Extreme caution should be exercised if using the puncture to advance large bore sheaths/devices.
Complications
Complications are higher in patients who have procedures done while being anticoagulated. The most dreaded complication is pericardial effusion or tamponade. This happens when the puncture is in the atrial wall through the superior/posterior muscular part of the septum into the left atrium, or when it is too anterior into the aorta.
- If a pericardial effusion develops immediately after TSP, the rate of progression should be monitored. If the effusion remains small, it can be monitored.
- If the effusion grows, emergent pericardiocentesis is warranted and the reversal of anticoagulation is recommended.
- If only the needle has been advanced, wire access can be maintained until hemodynamic stability is ensured.
- If the sheath has been advanced, it is maintained in position till surgical repair is done, or in a minority of cases, an occluder can be implanted to try and close the inadvertent track.
- Cardiac surgery should be on standby for surgical repair in case of progression of effusion/tamponade despite management in the catheterization lab.
Summary
- An imaging-guided TSP is the usual standard for interventions involving large bore systems in the current era.
- Proceduralists should be facile with understanding TEE and ICE landmarks for TSP.
- Troubleshooting a difficult TSP with appropriate steps is key to avoiding a life-threatening complication.
- In case of a complication, the operator should recognize the need to maintain wire/sheath access.
References
- Salghetti, F, Sieira J, Chierchia, G-B, et al. Recognizing and reacting to complications of trans-septal puncture. Expert Rev Cardiovasc Ther. 2017 Dec;15(12):905-912.
- Alkhouli, M, Rihal CS, Holmes, Jr, DR. Transseptal Techniques for Emerging Structural Heart Interventions. JACC Cardiovasc Interv. 2016 Dec 26;9(24):2465-2480.
- Guo, Q, Sang, C, Bai, R, et al. Transseptal puncture in patients with septal occluder devices during catheter ablation of atrial fibrillation. EuroIntervention. 2022 Jan 28;17(13):1112-1119.
Figure 1: Positioning of the trans-septal sheath and needle in RAO and LAO projections (reproduced with permission from Alkhouli , M, Rihal CS, Holmes, Jr, DR. Transseptal Techniques for Emerging Structural Heart Interventions. JACC Cardiovasc Interv. 2016 Dec 26;9(24):2465-2480).
Figure 2: (A) transseptal puncture with tenting in the bicaval view; (B) orthogonal plane in the short axis showing a posterior puncture for a MitraClip procedure
Figure 3: Transseptal puncture using intracardiac echocardiographic guidance – (A) visualization of the septum in the long axis; (B) tenting confirmed in the middle of the septum; (C) transseptal sheath visualized in the left atrium (reproduced with permission from Alkhouli, M, Rihal CS, Holmes, Jr, DR. Transseptal Techniques for Emerging Structural Heart Interventions. JACC Cardiovasc Interv. 2016 Dec 26;9(24):2465-2480).
Figure 4: Balloon dilation of the interatrial septum with a peripheral balloon – (A) a visible waist in the balloon; (B) resolution of the waist after a few inflations which facilitated crossing of the trans-septal sheath
Related QI Tips
Other evidence-based methods and tools you can use to improve quality of care and outcomes for patients.