ORLANDO (November 5, 2021) – A newly-developed expert consensus statement will provide updated guidance on the use of the SCAI SHOCK Stage Classification, a five-stage system intended to facilitate communication about the diagnosis, presentation, and evolving nature of cardiogenic shock (CS). A preview of the updated classification was presented live at 9 am EST on Friday, November 5 by Srihari S. Naidu, MD, Director of the Cardiac Catheterization Laboratory at Westchester Medical Center and Trustee of SCAI, during a featured session titled New Directions in Cardiogenic Shock at the 33rd annual Transcatheter Cardiovascular Therapeutics (TCT) conference. The document was developed in collaboration with the American College of Cardiology, American College of Emergency Physicians, American Heart Association, European Society of Cardiology Association for Acute Cardiovascular Care, Cardiac Safety Research Consortium, Society of Critical Care Medicine, and the Society of Thoracic Surgeons, each of which had representation on the writing group.
Cardiogenic shock (CS) is a serious and life-threatening condition that occurs when the heart is unable to pump enough blood to the body’s vital organs and is most commonly triggered by heart attack or heart failure. Mortality from cardiogenic shock complicating MI remains high, approaching or exceeding 50%, despite the development of percutaneous mechanical circulatory support technologies and the national standard of emergent angioplasty and stenting.
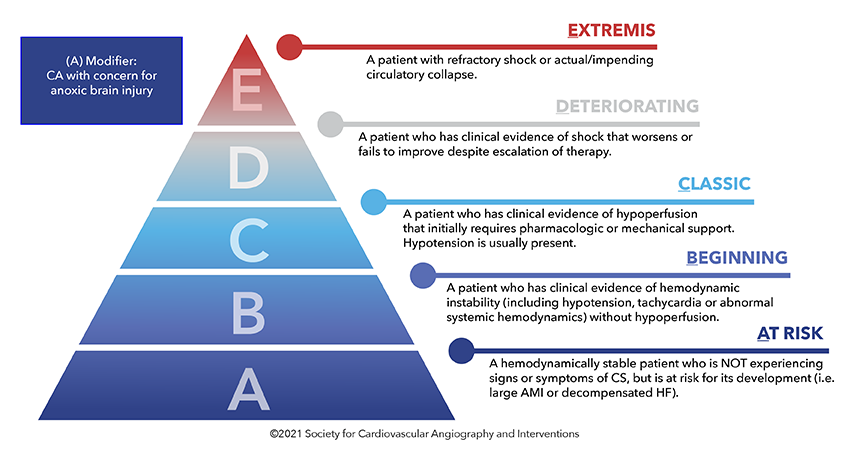
SCAI developed and released the SHOCK Stages classification in 2019 to provide a unified and standardized vocabulary that would translate across settings and providers from emergency room physicians and emergency medical services, to critical care physicians, heart failure physicians, interventional cardiologists, and surgeons. While the system has been widely adopted for its simple and intuitive framework, and ability to discern gradations of severity of CS for the first time, recent validation studies conducted since 2019 have uncovered areas in need of refinement.
“Studies continue to validate the SCAI SHOCK Stage classification as a tool to help clinicians and researchers better understand cardiogenic shock and offer guidance on treatment pathways to improve survival,” said Timothy Henry, MD, MSCAI, president of SCAI and Vice Chair of the Writing Group. "The updated expert consensus will underscore the benefit of the classification system across a broad patient spectrum and provides meaningful changes that we believe will enhance both clinical care and future research.”
Key points and highlights of the updated classification include:
- SCAI SHOCK Stage is an indication of shock severity and comprises one component of mortality risk prediction in CS patients, along with etiology/phenotype and other risk modifiers; a 3-axis model of risk stratification in CS has been proposed to position SCAI SHOCK Stage in context.
- Validation studies have underscored the correlation of SCAI SHOCK Stage with mortality across all clinical subgroups, including CS with and without acute coronary syndrome, cardiac intensive 20 care unit (CICU) patients, and those presenting with out-of-hospital cardiac arrest (OHCA). 21
- Progression across the SCAI SHOCK stages continuum is a dynamic process, incorporating new information as available, and patient trajectories are important both for communication among clinicians and for decision-making regarding the next level of care and therapeutics.
- A hub and spoke model for transfer of higher risk patients including those with deteriorating SCAI SHOCK Stage has been proposed
- Cardiac arrest (CA) as described herein relates to that accompanied by coma, defined as the inability to respond to verbal stimuli, most commonly associated with Glasgow Coma Scale < 9, where there is concern for significant anoxic brain injury.
- The SCAI SHOCK pyramid and associated figure now reflect gradations of severity within each stage and pathways by which patients progress or recover.
- A streamlined table incorporating variables that are most typically seen, and the revised CA modifier definition, is also provided and incorporates lessons learned from validation studies and clinician experience.
- Lactate level and thresholds have been highlighted to detect hypoperfusion but may be dissociated from hemodynamics in cases such as chronic heart failure. In addition, patients may demonstrate other manifestations of end-organ hypoperfusion with a normal lactate level and there are also important causes of an elevated lactate level other than shock.
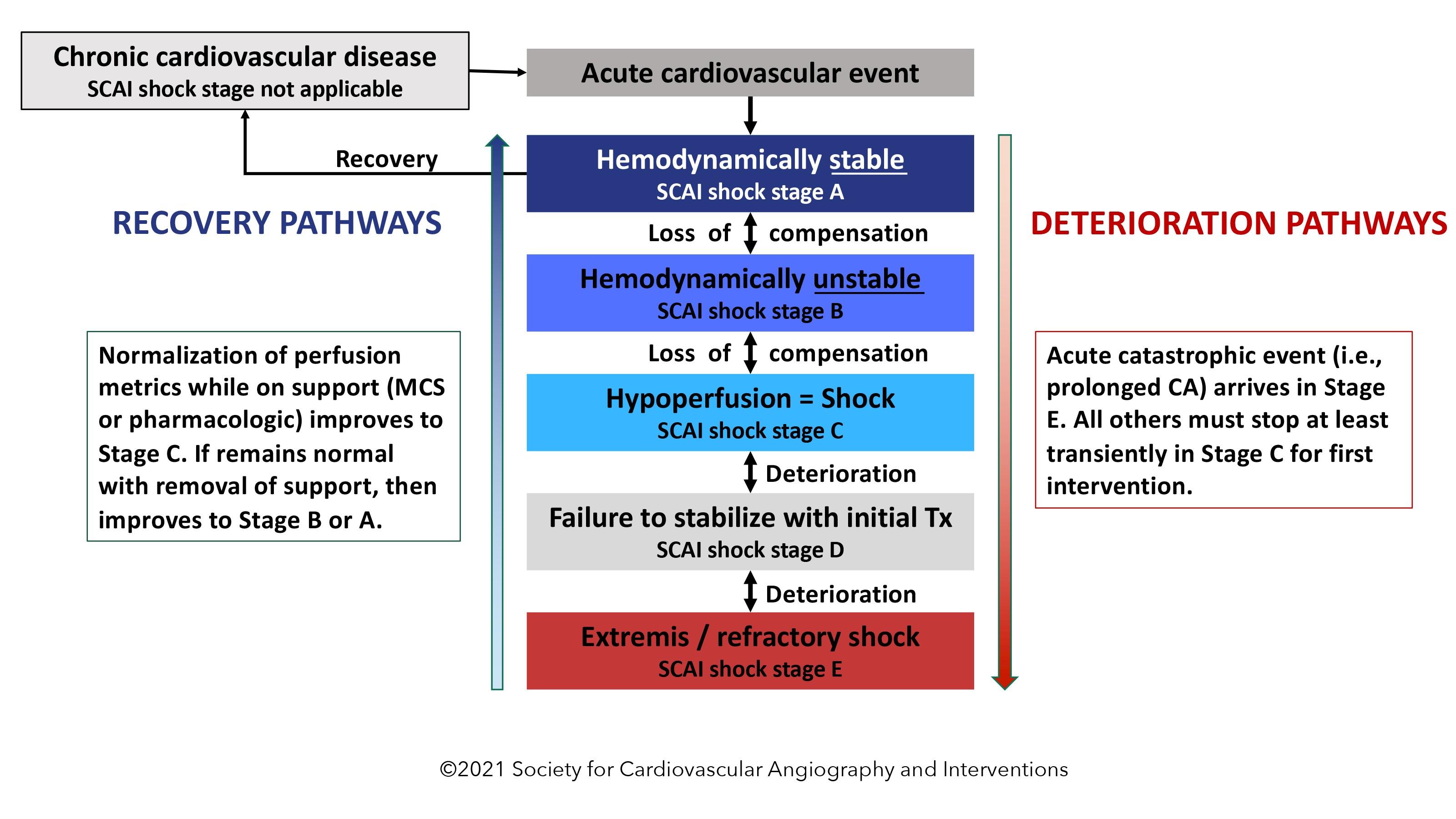
"The new Figures and updated Table should leave less room for interpretation and enhance the standardization significantly, including placing the SCAI SHOCK Stages in context with other variables that must be evaluated when managing a patient with CS”, states Dr. Naidu, who Chaired the Writing Group as well as the original one in 2019. “We also highlight new lactate thresholds and provide needed clarification for the pivotal SCAI SHOCK Stage C and the cardiac arrest modifier.”
The writing group was organized to ensure a diversity of perspectives and stakeholder representation and achieve multi-specialty consensus around the updated classification scheme.
SCAI anticipates publication of the manuscript in the coming months.
About SCAI:
The Society for Cardiovascular Angiography and Interventions is a professional organization representing more than 4,000 invasive and interventional cardiology professionals in approximately 75 nations. SCAI's mission is to promote excellence in invasive/interventional cardiovascular medicine through physician education and representation, and advancement of quality standards to enhance patient care.
What's New in Interventional Cardiology
Ground-breaking stories about what's happening in the field.

