Tamara Atkinson, MD; Jayant Bagai, MD, FACC, FSCAI; Faisal Latif MD, FSCAI
In-stent restenosis (ISR), defined as >50 percent diameter stenosis, accounts for about 10 percent of all percutaneous coronary interventions (PCIs) according to the National Cardiovascular Data Registry (NCDR).1 While rates of ISR have declined with the use of drug-eluting stents (DESs), the optimal treatment for DES-ISR remains unknown. Several techniques are available for the treatment of ISR, but not all therapies are available for commercial use in the United States such as drug-coated balloons (DCBs). The preferred therapy for bare-metal stent (BMS) ISR is DES implantation, a Class I indication according to the American College of Cardiology (ACC)/American Heart Association (AHA) guidelines; however, recurrent restenosis rates range from 10–30 percent.2–5 Recurrent ISR, defined as restenosis occurring after the implantation of ≥2 stents, remains a challenge with limited data regarding optimal therapy. This SCAI Tip of the Month focuses on tips and tricks to help with the management of ISR in the DES era.
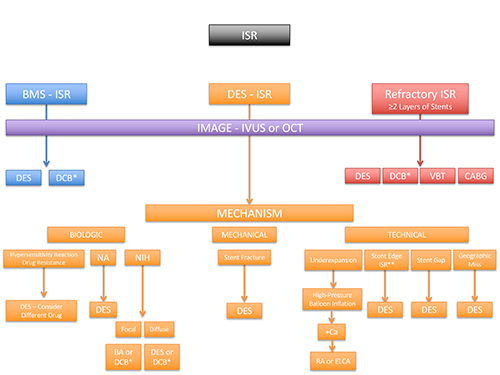
*Not FDA approved for use in the United States
**Secondary to barotrauma, edge dissection, or oversized stent on initial stent implantation
ISR—in-stent restenosis, DES—drug-eluting stent, BMS—bare-metal stent, DCB – drug-coated balloon, VBT – vascular brachytherapy, CABG – coronary artery bypass graft surgery, NA—neoatherosclerosis, NIH—neointimal hyperplasia, Ca—calcium, BA—balloon angioplasty, RA—rotational atherectomy, ELCA—excimer laser coronary angioplasty
- Define the pattern of ISR. BMS and DES have different patterns of ISR. BMS-ISR, classified by Mehran et al, tends to be diffuse and is predominantly due to neointimal hyperplasia (NIH).6 DES-ISR tends to be focal, secondary to both NIH and neoatherosclerosis (NA).7
- Image — identify the underlying mechanism. All in-stent luminal loss is not due to restenosis. It is possible the stent is undersized and/or underexpanded. Intravascular ultrasound (IVUS) or optical coherence tomography (OCT) can be used to determine the presence of underexpansion, NIH, NA, and calcification, thus guiding the appropriate treatment modality, as outlined in Figure 1.
- Know your techniques and when to use them in the management of ISR. In general, DESs for the treatment of ISR demonstrate superior results compared to balloon angioplasty, BMS, or brachytherapy.2–4 While DCBs demonstrate favorable results in the treatment of ISR without the addition of more metal, they are not available in the United States.8 Waksman et al proposed an algorithm for the treatment of ISR, which has been adapted in Figure 1.1
- Balloon angioplasty (BA) – BA should be performed for focal lesions, stent underexpansion, or if short dual antiplatelet therapy (DAPT) duration is favored. Balloon slippage, also known as “watermelon seeding,” is sometimes encountered during balloon inflation and can cause damage to the vessel wall. Tips to limit balloon slippage include the placement of a buddy wire, use of a noncompliant balloon, a shorter balloon length, slow inflation, or use of a scoring/cutting balloon.1 In the setting of stent underexpansion, high-pressure noncompliant balloon inflations are the preferred strategy.
- Scoring/cutting balloons – One trial demonstrated lower rates of restenosis with the use of a scoring balloon compared with a conventional balloon prior to a DCB.9 Scoring/cutting balloons help prevent balloon slippage, but their higher profile may limit deliverability.
- Rotational atherectomy (RA) – RA compared to BA has demonstrated mixed results for the treatment of ISR.10, 11 IVUS and OCT studies confirmed the presence of calcium within neoatherosclerotic plaques, and RA might be indicated for lesions refractory to high-pressure balloon inflation. Case series have also demonstrated the successful use of RA for undilatable underexpanded stents.12
- Excimer laser coronary angioplasty (ELCA) – ELCA is approved for the use in ISR by the U.S. Food and Drug Administration (FDA). Observational studies have demonstrated improved stent expansion facilitated by an ELCA with contrast injection in ISR, secondary to stent underexpansion refractory to high-pressure balloon inflation.13
- DCBs – Several trials and meta-analyses have demonstrated similar outcomes of DCBs compared to DESs in the management of ISR, with everolimus-eluting DESs coming out slightly ahead.14 While not available in the United States, the European Society of Cardiology (ESC)/European Association for Cardio-Thoracic Surgery (EACTS) guidelines give DCBs a class I indication for the treatment of ISR.15 DCB outcomes may be improved with prolonged inflation times >60 seconds and a balloon:artery ratio >0.91.16 DCBs may also play a role in recurrent ISR, but more investigation is needed.
- Brachytherapy – Brachytherapy use declined after trials demonstrated superior outcomes with DESs for the treatment of BMS-ISR. However, brachytherapy has had a resurgence for recurrent ISR, with several observational and prospective trials recently published.17, 18 In the setting of recurrent DES-ISR, referral to a brachytherapy center can be considered.
- Coronary artery bypass graft (CABG) – In patients with risk factors for restenosis or recurrent ISR, referral for a CABG should be considered via a Heart Team approach.
- Saphenous vein graft (SVG) ISR – When recurrent ISR develops within an SVG, a DES or brachytherapy can be considered, but if feasible, PCI to the native vessel chronic total occlusion (CTO) may be a better option.19
Conclusion
Adequate lesion preparation, image guidance, and high-pressure balloon post-dilatation during initial stent implantation should be standard to prevent ISR. However, if restenosis occurs, the majority of ISR should be treated with DES implantation. Optimal therapy for recurrent ISR is unknown and includes repeat DESs with or without a different drug, brachytherapy, or DCBs.
References
- Waksman R and Iantorno M. Refractory In-Stent Restenosis: Improving Outcomes by Standardizing Our Approach. Curr Cardiol Rep. 2018;20:140.
- Alfonso F, Perez-Vizcayno MJ, Hernandez R, Bethencourt A, Marti V, Lopez-Minguez JR, Angel J, Mantilla R, Moris C, Cequier A, Sabate M, Escaned J, Moreno R, Banuelos C, Suarez A, Macaya C, and Investigators R-I. A Randomized Comparison of Sirolimus-Eluting Stent With Balloon Angioplasty in Patients With In-Stent Restenosis: Results of the Restenosis Intrastent: Balloon Angioplasty Versus Elective Sirolimus-Eluting Stenting (RIBS-II) Trial. Journal of the American College of Cardiology. 2006;47:2152-60.
- Kastrati A, Mehilli J, von Beckerath N, Dibra A, Hausleiter J, Pache J, Schuhlen H, Schmitt C, Dirschinger J, Schomig A, and Investigators I-DS. Sirolimus-Eluting Stent or Paclitaxel-Eluting Stent vs Balloon Angioplasty for Prevention of Recurrences in Patients With Coronary In-Stent Restenosis: A Randomized Controlled Trial. JAMA. 2005;293:165-71.
- Mehilli J, Byrne RA, Tiroch K, Pinieck S, Schulz S, Kufner S, Massberg S, Laugwitz KL, Schomig A, Kastrati A, and Investigators I-D. Randomized Trial of Paclitaxel- Versus Sirolimus-Eluting Stents for Treatment of Coronary Restenosis in Sirolimus-Eluting Stents: The ISAR-DESIRE 2 (Intracoronary Stenting and Angiographic Results: Drug Eluting Stents for In-Stent Restenosis 2) Study. Journal of the American College of Cardiology. 2010;55:2710-6.
- Alfonso F, Perez-Vizcayno MJ, Dutary J, Zueco J, Cequier A, Garcia-Touchard A, Marti V, Lozano I, Angel J, Hernandez JM, Lopez-Minguez JR, Melgares R, Moreno R, Seidelberger B, Fernandez C, Hernandez R, and Investigators R-IS. Implantation of a Drug-Eluting Stent With a Different Drug (Switch Strategy) in Patients With Drug-Eluting Stent Restenosis. Results From a Prospective Multicenter Study (RIBS III [Restenosis Intra-Stent: Balloon Angioplasty Versus Drug-Eluting Stent]). JACC Cardiovasc Interv. 2012;5:728-37.
- Mehran R, Dangas G, Abizaid AS, Mintz GS, Lansky AJ, Satler LF, Pichard AD, Kent KM, Stone GW, and Leon MB. Angiographic Patterns of In-Stent Restenosis: Classification and Implications for Long-Term Outcome. Circulation. 1999;100:1872-8.
- Alfonso F, Byrne RA, Rivero F, and Kastrati A. Current Treatment of In-Stent Restenosis. Journal of the American College of Cardiology. 2014;63:2659-73.
- Kokkinidis DG, Prouse AF, Avner SJ, Lee JM, Waldo SW, and Armstrong EJ. Second-generation drug-eluting stents versus drug-coated balloons for the treatment of coronary in-stent restenosis: A systematic review and meta-analysis. Catheterization and Cardiovascular Interventions: Official Journal of the Society for Cardiac Angiography & Interventions. 2018;92:285-299.
- Kufner S, Joner M, Schneider S, Tolg R, Zrenner B, Repp J, Starkmann A, Xhepa E, Ibrahim T, Cassese S, Fusaro M, Ott I, Hengstenberg C, Schunkert H, Abdel-Wahab M, Laugwitz KL, Kastrati A, Byrne RA, and Investigators I-D. Neointimal Modification With Scoring Balloon and Efficacy of Drug-Coated Balloon Therapy in Patients With Restenosis in Drug-Eluting Coronary Stents: A Randomized Controlled Trial. JACC Cardiovasc Interv. 2017;10:1332-1340.
- Sharma SK, Kini A, Mehran R, Lansky A, Kobayashi Y, and Marmur JD. Randomized Trial of Rotational Atherectomy Versus Balloon Angioplasty for Diffuse In-Stent Restenosis (ROSTER). American Heart Journal. 2004;147:16-22.
- vom Dahl J, Dietz U, Haager PK, Silber S, Niccoli L, Buettner HJ, Schiele F, Thomas M, Commeau P, Ramsdale DR, Garcia E, Hamm CW, Hoffmann R, Reineke T, and Klues HG. Rotational Atherectomy Does Not Reduce Recurrent In-Stent Restenosis: Results of the Angioplasty Versus Rotational Atherectomy for Treatment of Diffuse In-Stent Restenosis Trial (ARTIST). Circulation. 2002;105:583-8.
- Ferri LA, Jabbour RJ, Giannini F, Benincasa S, Ancona M, Regazzoli D, Mangieri A, Montorfano M, Colombo A, and Latib A. Safety and efficacy of rotational atherectomy for the treatment of undilatable underexpanded stents implanted in calcific lesions. Catheterization and Cardiovascular Interventions: Official Journal of the Society for Cardiac Angiography & Interventions. 2017;90:E19-E24.
- Latib A, Takagi K, Chizzola G, Tobis J, Ambrosini V, Niccoli G, Sardella G, DiSalvo ME, Armigliato P, Valgimigli M, Tarsia G, Gabrielli G, Lazar L, Maffeo D, and Colombo A. Excimer Laser LEsion Modification to Expand Non-Dilatable Stents: The ELLEMENT Registry. Cardiovasc Revasc Med. 2014;15:8-12.
- Alfonso F, Perez-Vizcayno MJ, Cardenas A, Garcia del Blanco B, Garcia-Touchard A, Lopez-Minguez JR, Benedicto A, Masotti M, Zueco J, Iniguez A, Velazquez M, Moreno R, Mainar V, Dominguez A, Pomar F, Melgares R, Rivero F, Jimenez-Quevedo P, Gonzalo N, Fernandez C, Macaya C, and Investigators RIS. A Prospective Randomized Trial of Drug-Eluting Balloons Versus Everolimus-Eluting Stents in Patients With In-Stent Restenosis of Drug-Eluting Stents: The RIBS IV Randomized Clinical Trial. Journal of the American College of Cardiology. 2015;66:23-33.
- Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Juni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO, and Group ESCSD. 2018 ESC/EACTS Guidelines on Myocardial Revascularization. Eur Heart J. 2019;40:87-165.
- Rhee TM, Lee JM, Shin ES, Hwang D, Park J, Jeon KH, Kim HL, Yang HM, Han JK, Park KW, Hahn JY, Koo BK, Kim SH, and Kim HS. Impact of Optimized Procedure-Related Factors in Drug-Eluting Balloon Angioplasty for Treatment of In-Stent Restenosis. JACC Cardiovasc Interv. 2018;11:969-978.
- Varghese MJ, Bhatheja S, Baber U, Kezbor S, Chincholi A, Chamaria S, Buckstein M, Bakst R, Kini A, and Sharma S. Intravascular Brachytherapy for the Management of Repeated Multimetal-Layered Drug-Eluting Coronary Stent Restenosis. Circ Cardiovasc Interv. 2018;11:e006832.
- Negi SI, Torguson R, Gai J, Kiramijyan S, Koifman E, Chan R, Randolph P, Pichard A, Satler LF, and Waksman R. Intracoronary Brachytherapy for Recurrent Drug-Eluting Stent Failure. JACC Cardiovasc Interv. 2016;9:1259-65.
- Brilakis ES, Rao SV, Banerjee S, Goldman S, Shunk KA, Holmes DR, Jr., Honeycutt E, and Roe MT. Percutaneous Coronary Intervention in Native Arteries Versus Bypass Grafts in Prior Coronary Artery Bypass Grafting Patients: A Report From the National Cardiovascular Data Registry. JACC Cardiovasc Interv. 2011;4:844-50.
Related QI Tips
Other evidence-based methods and tools you can use to improve quality of care and outcomes for patients.
